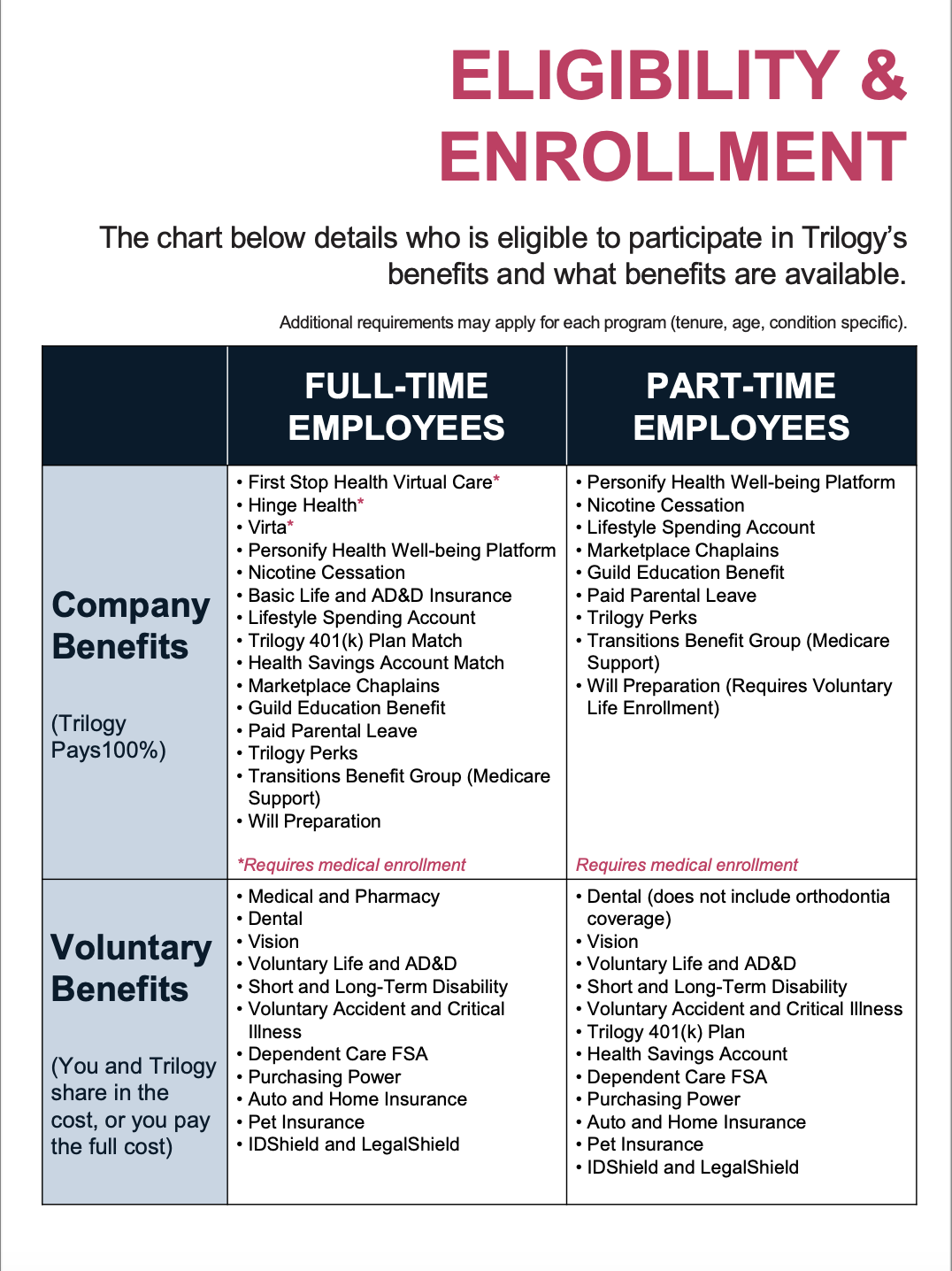
see who’s eligible
Part-time, full-time, benefits all the time.
We want to help you reach your goals, no matter what path you’re on. That’s one reason we offer such a long list of benefits. Also, our success depends on your success – and we like to dream big.

Let’s break down the benefits.
Whether you’re pulling long shifts or balancing part-time hours, there are plenty of perks to get excited about. What’s available depends on your employment status.
Don’t wait too long!
You have a limited window of time to take advantage of enrollment opportunities. So you need to take action fast – like 30 days fast. Keep reading to find what applies to you.
First of all, congrats! A whole world of great benefits and programs awaits you. And if you’re new to the company, well … welcome to the team!
Here’s what’s ahead of you:
- You have 30 days from your hire date or date of status change (for example, you’re moving from part-time to full-time) to enroll in major benefits (such as medical, dental and vision coverage) for the calendar year. Don’t miss your window for the benefits in this section!
- Go to the Enroll or Change Coverage page.
If you’re hired on or after October 1, or gain eligibility between October 1 and December 1, you’ll need to complete two enrollment periods:
- The first is for coverage during the current plan year.
- The second is for coverage beginning January 1 of the next plan year.
You’ll be walked through all these steps during your onboarding session
Got questions? We got you. The Benefits Resource Center is your best friend. Contact them at 888-350-0532 or by clicking here to get help.
It happens once a year, every October 1 – 15. That’s your chance to choose your coverage for all the plans in this Benefits Base Camp section.
- Note the dates of Open Enrollment. You’ll see plenty of posters and emails about it to get your attention.
- Check out each of the plans for details to help you make an informed decision.
- Use the Benefit Guide to help you see what’s changing in the new plan year along with the highlights of each coverage option available to you. You can access it here or see it in UKG, as well.
- Go to the Enroll or Change Coverage page to see how to make your selections.
And please, please, please: Don’t. Be. Late. Employees who miss the window to enroll CANNOT request changes after the enrollment window has ended.
Had some big life changes, like marriage or kids?
OK! That means you may be eligible to make mid-year coverage changes. Otherwise, you will need to wait until Open Enrollment. Also, be sure to check out our Life Journeys pages when you have time. You may find some additional benefits you didn’t know about.
To change your plan between annual enrollment periods, you must experience a Qualifying Life Event, or QLE.
Common events include:
- Marriage
- Divorce
- Birth
- Adoption
- Change in eligibility
How to Report a QLE
Login to your UKG account and head to the Benefits section.
Click the Declare an event button on the Report a Qualifying Change tile in UKG to register the event.
The date of the Qualifying Life Event must be the actual date of the event (marriage date or birth date, for example). Now you can move ahead with making your elections.
You have 30 days from the date of the Qualifying Life Event to register the event in UKG.
Contact the Benefits Resource Center at 888-350-0532 or by clicking here for help.
Your eligible family members include your:
- Legal spouse (can be added to your medical plan if they do not have medical coverage available from their employer or are unemployed)
- Children under 26 years old
- Children 26 or older if they are incapacitated due to a disability
Do you want to cover family members? Proof of eligibility is required.
- Once you’ve completed your enrollment and added family members to your coverage, UKG will send you a letter with details on the required documentation and submission deadline for verifying their eligibility.
- You must provide the documentation within 30 days of completing the QLE in UKG or the coverage you selected will be denied.
- Since your coverage becomes effective on the date of your Qualifying Life Event (QLE) once approved, you are responsible for any premium payments incurred between the QLE date and the date it was reported.
Questions right now? Contact the Benefits Resource Center at 888-350-0532 or by clicking here for help.
Have you recently lost coverage due to a change in your eligibility?
Coverage through COBRA might be a solution. You may be able to pay to keep your medical, dental and/or vision coverage for a limited time – even after your eligibility changes.
You may be eligible for COBRA coverage if:
- Your hours are reduced
- You terminate from the company
- You become Medicare eligible
- Your dependent ages out at 26 years old
To avoid any disruptions to your benefits and to receive important updates, please double-check that your details in UKG are accurate. This includes your social security number, home address, email, phone number and date of birth for you and any dependents (if applicable).
Wage Works/HealthEquity will mail a packet of information to your home, typically within 7-10 business days of when your change in eligibility has been entered into our HR system. This will include pricing and paperwork.
